From the SIR Residents and Fellows Section (SIRRFS) Teaching Topic: Uterine Artery Embolization for the Treatment of Adenomyosis: A Systematic Review and Meta-Analysis
de Bruijn AM, Smink M, Lohle PN, Huirne JA, Twisk JW, Wong C, Schoonmade L, Hehenkamp WJ. Uterine Artery Embolization for the Treatment of Adenomyosis: A Systematic Review and Meta-Analysis. Journal of Vascular and Interventional Radiology. 2017 Oct 9.
Click here for abstract This evidence-based review article evaluated the effect of uterine artery embolization (UAE) on symptom reduction in adenomyosis with respect to length of follow-up (< 12 months or >12 months) and whether patients had pure (adenomyosis alone) or combined (adenomyosis and fibroids) disease. The meta-analysis supported that uterine artery embolization (UAE) for both pure and combined adenomyosis resulted in significant short-term and long-term symptom improvement. There were limitations in that no randomized controlled trials were available, many included studies were retrospectively evaluated, many studies had a small sample size, and many studies offered vague description of methodology. As well, the sample size of most included studies was not sufficient to draw solid conclusions. This called for future trials to use standardized outcomes and validated questionnaires to render outcomes that can be extrapolated in systematic reviews.
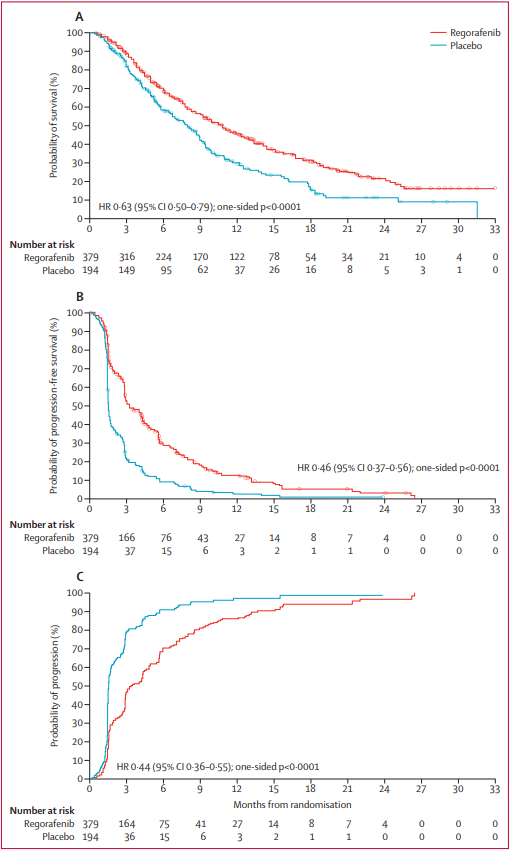
 Figure.
Figure. Improvement of clinical symptoms (%).
Clinical Pearls
What is the pathophysiology of adenomyosis? Adenomyosis defined as heterotopic endometrium in the myometrium and has diffuse, segmental, superficial, and deep forms. It is typically considered a disease of multiparous women in the late reproductive years. Though the etiology is still not well known, adenomyosis is thought to occur from either endomyometrial invagination of the endometrium or de novo from mullerian rests. There is also evidence that the junctional zone (JZ), which separates the subendometrial myometrium from the outer myometrium (appears as a dark band on T2WI), plays a role, as disease in the JZ predisposes to secondary infiltration of endomyometrial elements. Aside from older, multiparous women, JZ distortion can also be found in young, nulliparous women with heavy periods. A JZ > 12 mm is highly predictive of disease and < 8 mm essentially excludes it. Six studies in the meta-analysis reported a JZ reduction of 13.7%-38% after UAE. Smeets et al reported a thicker JZ at baseline to be a possible predictor of UAE failure in patients with adenomyosis. Patients who underwent hysterectomy owing to persisting symptoms compared with patients with clinical improvement showed a statistically significant thicker JZ at baseline (P = .028) and during 3 months (P = .034) of follow-up. Nijenhuis et al reported the mean JZ thickness at baseline not to be significantly thicker in groups with insufficient response (P = .17); however, it was statistically significant thicker in 4 patients needing additional therapy (P = .004).
What other gynecological pathologies are associated with adenomyosis?
Concurrent benign, estrogen-dependent gynecologic pathology, namely leiomyoma and endometriosis, is often present, increasing operative risks for major gynecologic surgery. There is also a known association between recurrent fetal loss and adenomyosis, though there is no direct evidence that adenomyosis is a risk factor for spontaneous abortion. The authors of this study state that in addition to the use of standardized outcomes and validated questionnaires, future trials should focus on fertility results in patients with symptomatic adenomyosis. Only two of the thirty-four studies in their meta-analysis reported fertility outcomes in terms of pregnancy outcome after UAE. Kim et al reported on 5 pregnancies. Two of these patients underwent elective abortion owing to unwanted pregnancies. The remaining three patients carried to term and showed no signs of uteroplacental vascular insufficiency or abnormal uterine contraction during labor or postpartum. The pregnancies resulted in 2 vaginal deliveries and 1 elective cesarean delivery because of previous cesarean delivery. The average weight of neonates was 3.2 kg (range, 3.1–3.4 kg). Yao et al described 1 pregnancy after UAE reporting termination of the pregnancy after 26 weeks. The reason for termination was not reported. Of 99 patients, 6 (6%) became pregnant after UAE. There is a paucity of high-quality data documenting the ability to conceive following UAE. Studies have reported between 48-59% live birth pregnancy rates, although the data is limited and influenced by age and current fertility status. Based on limited data, a discussion should take place with the patient about her fertility goals and a referral to a reproductive endocrinologist may also be helpful.
Why are symptoms of adenomyosis?
Though adenomyosis may be asymptomatic, it typically produces the symptoms of dysmenorrhea, dyspareunia, and chronic pelvic pain. These are also the most common symptoms of the other estrogen-dependent, benign gynecologic pathologies of endometriosis, leiomyoma, and endometrial polyp, which makes delineation of the symptoms profile difficult if the processes are concurrent. The included studies in this meta-analysis reported improvement of clinical symptoms in 83.1% (872 of 1,049) of patients. Only five of the thirty-four studies used the standardized Uterine Fibroid Symptom and Quality of Life (UFS-QOL; Spies JB, Coyne K, Guaou Guaou N, Boyle D, Skyrnarz-Murphy K, Gonzalves SM. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol 2002; 99:290–300) questionnaire to evaluate health-related quality of life (HRQOL) and symptom severity. This use of this questionnaire should be used in future trials to render outcomes that can be extrapolated in systematic reviews.
Question to Consider
What are complications of UAE?
There were 20 studies that reported on complications in 615 patients. Abdominal pain occurring directly following the procedure until 2 weeks after the procedure was described in 361 of 413 patients (87.4%). Persistent amenorrhea was reported in 28 of 445 patients (6.3%) in 13 studies. All of these patients were > 40 years of age. A pseudoaneurysm was reported, which was treated with a thrombin injection. Spontaneous expulsion of leiomyomata was reported in ten patients. Endometritis was suspected in four patients. These patients were treated with broad-spectrum antibiotics. Deep venous thrombosis of the calf occurred in one patient; however, this patient did not require anticoagulation therapy. No deaths or other complications occurred.
For pain control, patient controlled analgesia with IV morphine, meperidine, hydromorphone, or fentanyl is effective. Some interventionalists prefer epidural or oral administration of narcotics. UAE patients often suffer nausea post-procedure and require either prophylactic administration or, as needed, delivery of antiemetic such as odansetron. Anti-inflammatory agents such as IV ketorolac or oral ibuprofen periprocedurally or postoperatively are commonly used. Some physicians prefer administering steroids pre-procedurally, as well, to help limit post-embolization symptoms.
The risk of infection in UAE is low with reported rates of 0.2-1% of patients. Infection usually occurs in a delayed fashion, one to two weeks after the procedure. There have been several cases of fatal sepsis occurring after UAE in patients who did not receive prophylactic antibiotics. Currently, SIR recommends prophylaxis with a single dose of 1 mg Cefazolin IV as a common choice to cover typical organisms causing infection, including skin flora and E. Coli
1. Genc M, Genc B, Cengiz H. Adenomyosis and accompanying gynecological pathologies. Arch Gynecol Obstet 2015; 291:877–881.
Brosens JJ, de Souza NM, Barker FG. Uterine junctional zone: function and disease. Lancet 1995; 346:558.
3. Spies JB, Coyne K, Guaou Guaou N, Boyle D, Skyrnarz-Murphy K, Gonzalves SM. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol 2002; 99:290–300.
4. LoVerme W, James M, Ho Ahn S. “Patient Evaluation: Genitourinary System.” Patient Care in Vascular and Interventional Radiology. Third Edition. Society of Interventional Radiology, 2016. 99-111. Print.
Post Author:
Rajat Chand
Radiology Resident
John H. Stroger, Jr. Hospital of Cook County