Stability of Retained Inferior Vena Cava Filter Fragments after Filter Removal
Clinical question
How stable are retained IVC filter fragments over time?
Take away point
Take away point
98% (50/51) retained IVC filter components were stable in position by imaging at a mean imaging time of 875 days (note the single filter component deemed unstable never embolized; it rotated 180 degrees from its intramuscular position and was therefore felt to be “unstable”). The findings suggest that IVC filter fragments are predominantly stable over time.
Reference
Puller, H. F., Stavropoulos, S. W., & Trerotola, S. O. (2021). Stability of Retained Inferior Vena Cava Filter Fragments after Filter Removal. Journal of Vascular and Interventional Radiology, 32(10), 1457-1462.
Single center retrospective
Funding source
Funding source
No reported funding
Setting
Setting
Hospital of the University of Pennsylvania
Figure
Figure
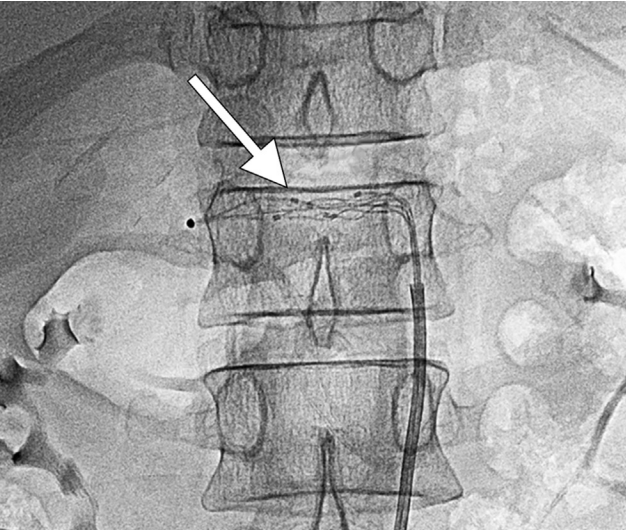
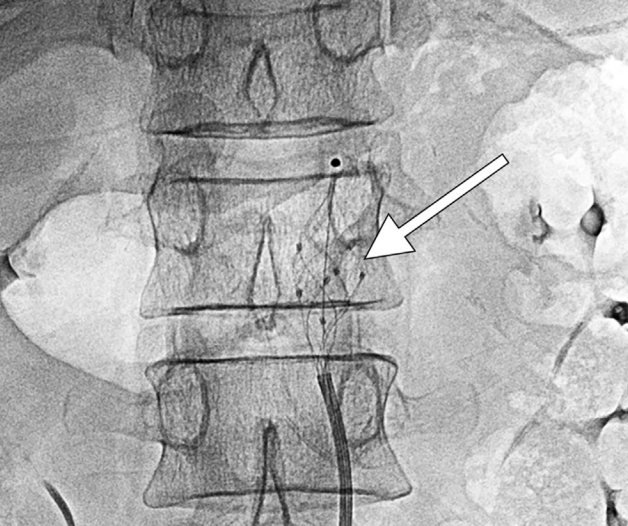
Figure 1(a) Initial computed tomography imaging of a single unstable fragment (leg) located in the right psoas muscle. The fragment concavity can be seen facing laterally (white arrow). (b) The 34-month follow-up X-ray imaging displaying interval rotation of the same fragment. The concavity can now be seen facing posteromedially (white arrow).
In 2010 there was a safety communication from the FDA due to reports of IVC filter migration and component fracture/embolization. The recommendation at the time was to consider removal of all IVC filters, if possible, once the risk of pulmonary embolism had been mitigated. The safety communication was updated in 2014 to again report the risks of IVC filter component fracture, as well as to update providers with data that IVC filter benefit was now felt to decrease at dwell times greater than 54 days.
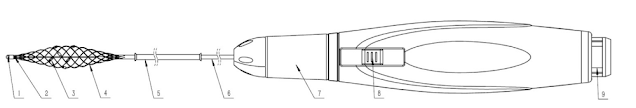
The group of authors of the current study have previously discussed retrieval of IVC filter components in 2017. In that study, a retrospective analysis spanning 11 years. 65 patients were identified who had 116 different filter components which were fractured. The authors were able to remove 81% of the fragments that they targeted (primarily using endobronchial forceps), however, the overall removal rate of was only 54% (63/116) due to components that were not able to be targeted e.g extravascular or distal pulmonary artery. The study was useful in that it demonstrated that filter fragment retrieval could be performed safely and with high technical success. However, given that many of the filter components were left in situ, the stability of these malpositioned filter components over time remained unanswered.
The current study therefore aimed to answer that question. A retrospective review was performed at a single center from 2005 through 2020. The review identified 37 patients who presented for a complex filter removal. These individuals had fractured filter components at the time of referral which were either unable to be removed during the filter retrieval procedure, or, were not targeted for removal due to difficult or inaccessible locations. Patients were included in the review only if imaging was available at a minimum of 28 days after the last imaging of the fracture component.
In total the 37 patients had 51 total fractured filter components for review. Of the 51 components, the locations were as follows:
This study informs us that IVC filter components which are fractured are very likely to be stable over time. Most of the filter components in the study seemed to be embedded. For example, these components were ones that persisted despite prior attempts at removal with endobronchial forceps or, the components were in areas that no attempt at removal was even attempted e.g. the extravascular space or distal pulmonary arteries.
These findings indicate that we can reassure patients that retained extravascular IVC filter components, or filter material that is partially intravascular but embedded (resistant to advanced removal technique, including forceps), should be followed conservatively with imaging. The expectation is that these filter components will not migrate nor will they be clinically relevant in any way.
Lastly, the importance of IVC filter tracking and retrieval programs should be highlighted given the frequency of fracture which is the reason this study was needed in the first place.
Post Author
Robert Elliott, DO
Interventional Radiology Resident, PGY6
University of Rochester Medical Center, Rochester, New York
Summary
In 2010 there was a safety communication from the FDA due to reports of IVC filter migration and component fracture/embolization. The recommendation at the time was to consider removal of all IVC filters, if possible, once the risk of pulmonary embolism had been mitigated. The safety communication was updated in 2014 to again report the risks of IVC filter component fracture, as well as to update providers with data that IVC filter benefit was now felt to decrease at dwell times greater than 54 days.
The group of authors of the current study have previously discussed retrieval of IVC filter components in 2017. In that study, a retrospective analysis spanning 11 years. 65 patients were identified who had 116 different filter components which were fractured. The authors were able to remove 81% of the fragments that they targeted (primarily using endobronchial forceps), however, the overall removal rate of was only 54% (63/116) due to components that were not able to be targeted e.g extravascular or distal pulmonary artery. The study was useful in that it demonstrated that filter fragment retrieval could be performed safely and with high technical success. However, given that many of the filter components were left in situ, the stability of these malpositioned filter components over time remained unanswered.
The current study therefore aimed to answer that question. A retrospective review was performed at a single center from 2005 through 2020. The review identified 37 patients who presented for a complex filter removal. These individuals had fractured filter components at the time of referral which were either unable to be removed during the filter retrieval procedure, or, were not targeted for removal due to difficult or inaccessible locations. Patients were included in the review only if imaging was available at a minimum of 28 days after the last imaging of the fracture component.
In total the 37 patients had 51 total fractured filter components for review. Of the 51 components, the locations were as follows:
- Pericaval (extravascular): 20
- Pulmonary artery: 10
- Wall of IVC: 5
- Heart: 5
- Other: 11
Commentary
This study informs us that IVC filter components which are fractured are very likely to be stable over time. Most of the filter components in the study seemed to be embedded. For example, these components were ones that persisted despite prior attempts at removal with endobronchial forceps or, the components were in areas that no attempt at removal was even attempted e.g. the extravascular space or distal pulmonary arteries.
These findings indicate that we can reassure patients that retained extravascular IVC filter components, or filter material that is partially intravascular but embedded (resistant to advanced removal technique, including forceps), should be followed conservatively with imaging. The expectation is that these filter components will not migrate nor will they be clinically relevant in any way.
Lastly, the importance of IVC filter tracking and retrieval programs should be highlighted given the frequency of fracture which is the reason this study was needed in the first place.
Post Author
Robert Elliott, DO
Interventional Radiology Resident, PGY6
University of Rochester Medical Center, Rochester, New York
Edited and formatted by @NingchengLi
Interventional Radiology Resident
Dotter Institute, Oregon Health and Science University