Absolute Ethanol Embolization of Lip Arteriovenous Malformations: Observational Results from 10 Years of Experience
Clinical question
What is the safety and efficacy of lip arteriovenous malformation (AVMs) ethanol embolization via direct puncture or transarterial catheterization technique, with or without follow-up surgical resection?
Take away point
Lip AVM treatment remains variable. Ethanol embolization of lip AVMs in single or multiple sessions was able to achieve complete devascularization in 67% of the patients and complete cosmetic resolution in 53% of patients. When including preoperative embolization followed by surgical resection, 71% achieved complete cosmetic relief and all patients endorsed major to complete improvement of functional impairment.
Reference
Su LX, Li XY, Zhao ZJ, Shao YH, Fan XD, Wen MZ, Yang XT. Absolute Ethanol Embolization of Lip Arteriovenous Malformations: Observational Results from 10 Years of Experience. J Vasc Interv Radiol. 2022 Jan;33(1):42-48.e4. doi: 10.1016/j.jvir.2021.09.004. Epub 2021 Sep 20. PMID: 34547475.
Click here for abstract Study design
10-year retrospective, observational study of 76 patients
Funding source
(1) Fundamental research program funding of Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine (No. JYZZ076)
(2) Clinical Research Program of Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine (No. JYLJ201801 and JYLJ201911)
(3) China Postdoctoral Science Foundation (No. 2017M611585)
(4) National Natural Science Foundation of China (No. 81871458)
Setting Urban academic center at the Shanghai Ninth People’s Hospital which is affiliated with the Shanghai Jiao Tong University School of Medicine
Figures 
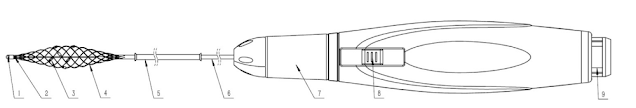
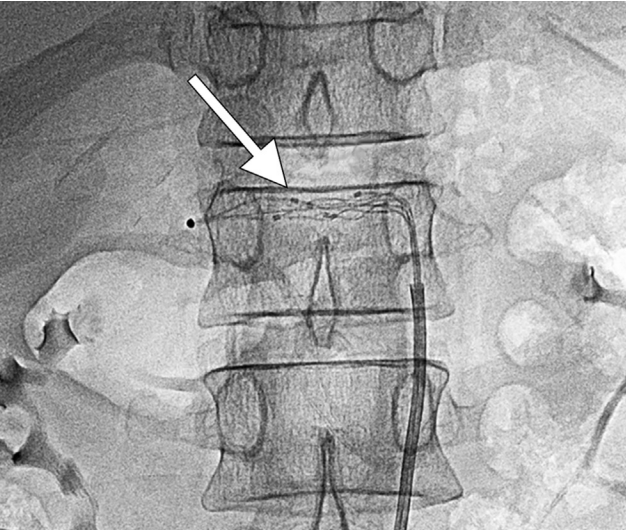
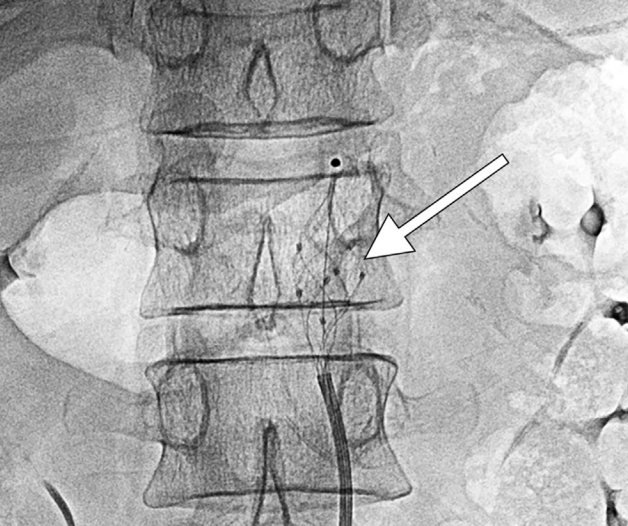
Figure 1: Intraprocedural digital subtraction angiography (DSA) of a 17-year-old male treated for a pulsating AVM. (a) A focal AVM nidus is opacified with contrast (arrow). (b) Lateral view demonstrates the 1.7 Fr microcatheter at the AVM nidus via superselective embolization from the facial artery. (c) Subsequently, direct 21-guage needle puncture was used to perform an additional embolization of the nidus. (d) The post-procedure lateral view DSA demonstrates 100% AVM devascularization.
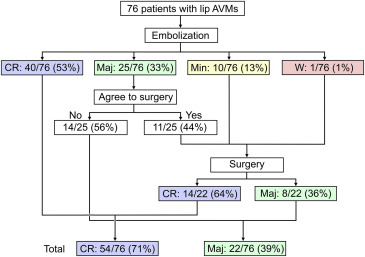
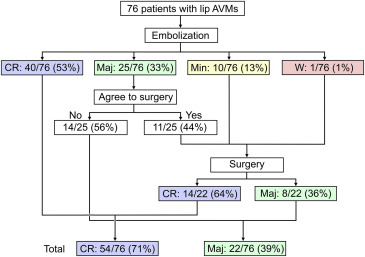
Figure 2: Of the 76 patients treated with embolization, most with multiple sessions, the majority went on to have complete cosmetic resolution either solely with ethanol embolization or after ethanol embolization and subsequent surgical resection, and 100% of patients endorses complete or major resolution of cosmetic appearance.
Summary
Lip arteriovenous malformations (AVM) may be present at birth and can enlarge over time secondary to trauma or hormonal changes. Radical surgical resection can result in functional/ cosmetic defects and may risk severe intraoperative hemorrhage. Incomplete resection fails to provide symptom relief. Thus, AVM embolization is increasingly becoming the treatment of choice.
This study utilized
ethanol as a permanent embolic agent. Other studies of peripheral AVM embolization have used
ethylene vinyl alcohol copolymer and
n-butyl cyanoacrylate (n-BCA) glue, however reports show
nidus recanalization can occur, and
subcutaneous accumulation of the embolic glue can cause infection. Ethanol injection permanently destroys the vascular endothelium by causing protein denaturation and nidus thrombosis. Downsides of ethanol embolization include risks of
systemic ethanol toxicity which can include cardiopulmonary arrest and disseminated intravascular coagulation (DIC).
This 10-year retrospective study includes patients with lip AVM Schobinger stage II or higher (growing or symptomatic AVM). Many patients had prior treatments (including surgical resection, sclerotherapy, propranolol, radiofrequency ablation and artery ligation), but only those at least 3 months post prior therapy were included. Other exclusion criteria included contrast or ethanol allergy and major cardiac, respiratory, renal or hepatic impairment.
Lip AVM embolization was performed under general anesthesia, with a Foley catheter in place to monitor for hemoglobinuria secondary to ethanol administration and arterial line for blood pressure monitoring. Pulmonary artery pressure was measured in those expected to have high ethanol volume administered.
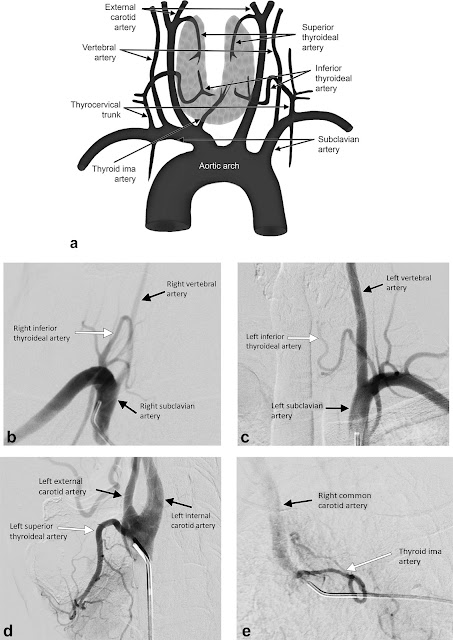
Digital subtraction angiography (DSA) was performed via superselective angiography of the external and internal carotid arteries using a 4 or 5 Fr catheter to identify the AVM nidus based on feeding vessels, draining veins, and internal blood flow. Then, a 1.7 Fr microcatheter was advanced into the nidus. If complete nidus access was not feasible by this technique alone, they performed ultrasound-guided direct puncture using a 21-guage butterfly needle.
If a draining outflow vein (DOV) was identified, it was coil-embolized prior to ethanol embolization. Required ethanol volume was estimated based on the amount of contrast injected to fill the AVM nidus. Usually 100% ethanol was used except in patients with a diffuse infiltrating AVM where diluted ethanol was used to reduce risks of systemic toxicity. In all cases,
less than 1 cc/kg of ethanol was used during each session, and staged embolization was used in patients to reduce risks of ethanol toxicity. Additionally,
manual pressure was applied around the target lesion to reduce non-target embolization.
The 76 patients enrolled underwent a mean of 2.3 procedures (range of 1-7 procedures) and were followed for a mean of about 2.5 years. Patients were asked to self-report cosmetic changes on a scale of 1-5 after treatment, and functional results were evaluated by oral maxillofacial surgeons.
Roughly 67% of patients had 100% AVM devascularization on arteriography. One third of patients had 76-99% devascularization and 26.3% experienced 50-75% devascularization. Symptomatically, 53% of patients had complete cosmetic improvement after embolization alone. A third of patients self-reported major cosmetic improvement, and 44% of them underwent surgery to see further improvement. Those who rated their cosmetic changes as minorly improved or worsened underwent surgery, all of whom felt they had major improvement or complete improvement postoperatively. In total, 71% had complete cosmetic resolution of their AVM and 39% had major cosmetic improvement with embolization alone or followed up by surgical resection.
Immediate post-procedure swelling was seen in almost all patients and resolved within 2 weeks. The most common complication was local skin bullae, which occurred in 9.2% of procedures and spontaneously resolved. There were
3 cases of skin necrosis, one of whom developed serious lip necrosis causing cosmetic deformity that required surgery.
Two patients developed transient hemoglobinuria which was treated with IV infusion. No severe complications were reported.
Commentary
The study is limited by its retrospective nature, potential for patient selection bias, relatively small sample size and nonstandardized treatment algorithm which included a mix of embolization, coil embolization of the draining vein when present, and postprocedural surgery. A randomized control trial with a placebo arm as well as comparative groups randomly assigned to surgical or embolization therapy would be useful. Additionally, comparing the efficacy and complications of other embolic materials and combination of coils or plugs would be advantageous for clinical decision-making. Although ethanol is highly effective, rare reports of systemic effects causing DIC and cardiopulmonary arrest may be a considerable drawback for centers that do not perform lip AVM commonly.
Future studies could consider enrolling treatment-naïve patients. In this study, more than half of the patients had prior laser treatment, sclerotherapy, radiofrequency ablation or arterial embolization, performed at least 3 months prior. This may confound the results of ethanol embolization, especially in cases of prior surgical resection or arterial ligation, which can complicate future embolization access. Additionally, the study on average followed patients for 2.5 years, and though ethanol embolization is permanent when injected, AVM recurrence may occur in untreated regions of a diffuse, infiltrating AVM beyond that time frame. Another limitation is that post-procedure cosmetic results were quantified based on a subjective patient-derived scale; however, this appears to have been used in prior studies.
In conclusion, the study authors convey that
lip AVM treatment can be challenging due to the nature of the AVM vascular anatomy, however multifactorial treatment options can produce acceptable results in most patients. Treatment options were customized throughout the course of therapy and tailored to patient preferences regarding cosmetic improvement. These options include multiple courses of ethanol embolization via
superselective angiography and/or direct puncture technique, post-procedure surgical resection, and draining outflow vein coil embolization. The study reports that most patients had complete or major improvement of cosmetic and functional symptoms and embolization and/or surgical resection. However, a subset of patients was not able to achieve complete resolution of their cosmetic defects despite multiple sessions of embolization and surgical resection, underscoring the
complicated treatment course of peripheral AVMs and the importance of accurately conveying to patients the realities of AVM treatment.
Post author
Surbhi B. Trivedi, MD
Diagnostic Radiology PGY-3 Resident
University of Illinois, Chicago
@surbhitrivedi3
Edited and formatted by @NingchengLi
Interventional Radiology Resident
Dotter Institute, Oregon Health and Science University