Endovascular Celiac Denervation for Glycemic Control in Patients with Type 2 Diabetes Mellitus
Clinical question
Can a novel method of endovascular denervation (EDN) by radiofrequency ablation of the celiac and peri-celiac aortic ganglionic sympathetic nerves improve glycemic control in patients with type II diabetes mellitus (DM2)?
Take away point
The investigators found a clinically significant improvement in glycemic control and insulin resistance in a small single-arm cohort of 11 patients with DM2 treated with endovascular denervation in the celiac artery and adjacent abdominal aorta, without any significant vascular or gastrointestinal complications. This is the first study in humans using this technology for the control and treatment of DM2.
Study design
Prospective, single-arm, non-randomized, proof-of-concept pilot study of 11 patients with DM2.
References
Pan T, Li L, Wei Q, Wang Z, Zhang Q, Qian Y, Li R, Liu DC, Wang Y, Sun ZL, Teng GJ. Endovascular Celiac Denervation for Glycemic Control in Patients with Type 2 Diabetes Mellitus. J Vasc Interv Radiol. 2021 Nov;32(11):1519-1528.e2. doi: 10.1016/j.jvir.2021.07.023. Epub 2021 Aug 6. PMID: 34364991.
Click here for abstract
Funding source
Academic research grants including:
National Major Program of Research and Development of China (2018YFA0704100)
Major Program of Scientific Instrument of the National Natural Science Foundation of China (81827805)
Clinical Medicine Center of Jiangsu Province (Innovation Section) (YXZXA2016005)
National Natural Science Foundation of Jiangsu Youth Project (BK20200365)
Setting
Academic hospital, Nanjing Drum Tower Hospital, Medical School of Nanjing University
Figures
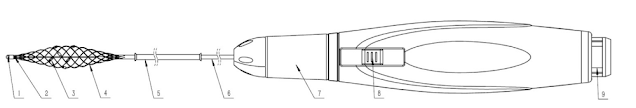
The novel single-use denervation catheter (Golden Leaf, Shanghai, China) with 6-electrodes is illustrated. The accessory RF generator is not shown. The catheter is composed of a central wire (1), mesh tube (2), electrodes (3), mesh stent (4), and a protective sheath (5). The catheter is first exposed, then deployed, after which the electrodes are apportioned to the blood vessel wall, and EDN is then performed.
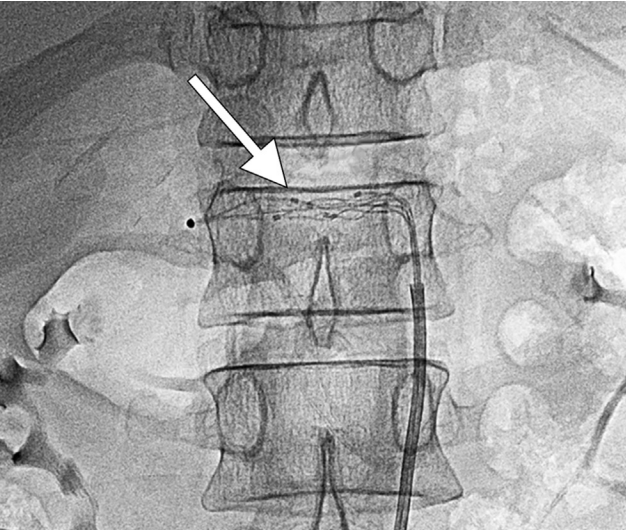
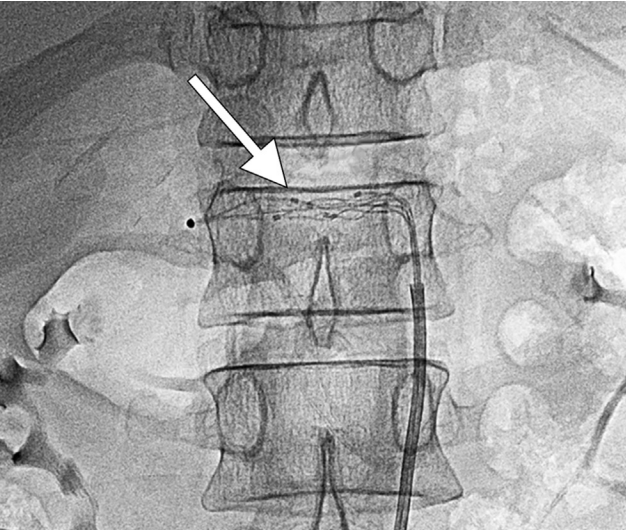
The denervation device is positioned in the celiac artery, where 1 cycle of RF ablation occurs.
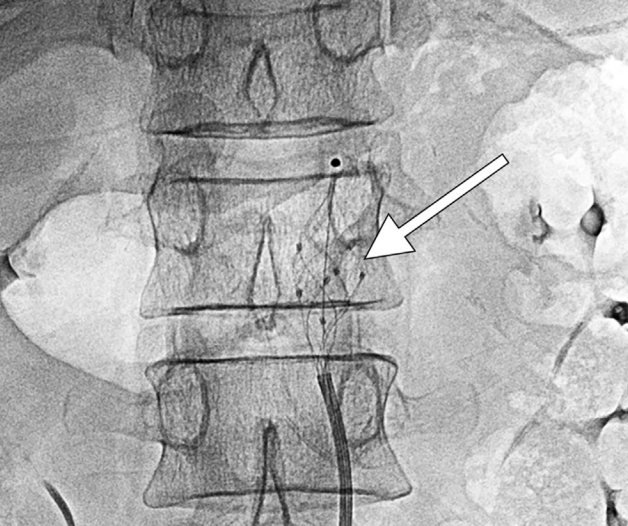
The denervation device is positioned in the aorta around the celiac artery, where 2 cycles of RF ablation occur.
The study enrolled 11 patients with DM2 seeking to improve glycemic control via endovascular denervation of the celiac and peri-celiac sympathetic postganglionic nerves, which suppresses insulin secretion from pancreatic β islet cells. This treatment methodology is based on animal study that showed improved glucose tolerance in rats after celiac ganglionectomy, as well as incidental clinical results in a subset of cancer patients treated with postganglionic nerve block who developed improved glycemic control. The study enrolled patients aged 18-75 with DM2 for at least 5 years, using at least one form of diabetic medication, with the majority of patients using insulin. A 6-electrode radiofrequency endovascular catheter was used to target and ablate the post-ganglionic sympathetic nerves at the celiac and superior mesenteric ganglia. Using a transfemoral approach, an aortogram was performed to position the catheter at the level of the celiac artery and superior mesenteric artery. The EDN device was then deployed, and allowed to ablate for 3 cycles of 120 seconds each at a temperature of 60 degrees Celsius, with a maximum impedance of 400 Ω, after which a completion arteriogram was performed to ensure no vascular injury.
All of the participants achieved technical success, and there were no cases of vascular injury. Approximately 36% of patients developed immediate arterial vasospasm, which resolved shortly thereafter, while a few others developed self-limiting nausea and vomiting, abdominal distention, or constipation. Six-month follow-up demonstrated a significant decrease in the mean HbA1c by 1.9% as well as a significantly decreased homeostasis model assessment of insulin resistance (HOMA-IR) from 13.3 (IQR 5.9-46.1) to 6.0 (IQR 3.1-11.9). Mean fasting plasma glucose also decreased, and 36.4% of patients were able to discontinue at least 1 class of diabetic medication. Weight and body mass index did not undergo significant change, however there was significant decrease in alanine aminotransferase (baseline mean 31.0 IU/L to 24.0 IU/L at 6 months) and gamma glutamyl transpeptidase levels (baseline mean 47.0 IU/L to 27.0 IU/L at 6 months). These reductions suggest an additional modulating effect of EDN on nonalcoholic fatty liver disease (NAFLD), consistent with a recent animal study showing that manipulation of hepatic sympathetic innervation may be a novel therapeutic strategy for NAFLD.
The Centers for Disease Control and Prevention estimates that nearly 1 in 10 Americans have diabetes, making it a disease with significant epidemiologic burden and many associated health complications. Thus, any novel treatment to alleviate this immense, growing public health burden could be hugely impactful. Endovascular denervation has been gaining traction in treating another prevalent disease, specifically resistant/refractory hypertension (HTN). This technique is a minimally invasive descendant of surgical sympathectomy for the same indication, which was promising but seemed overly invasive in the face of evolving pharmaceutical therapies. Thus far, results in randomized control trials of renal denervation (RDN) have been promising but mixed, some of which may be attributable to operator inexperience with the technique. Since hypertension and DM2 are frequently comorbid diseases, studies were able to assess the role of RDN in DM2 and showed early promise for achieving glycemic control. However further studies have not shown reliable success for denervation of the renal arteries.
This study by Pan et al. coopts this technique in a different anatomic location, the celiac and peri-celiac aorta, with early promising results as an endovascular approach to achieving glycemic control in patients with DM2. Given that this is a small, nonrandomized study without a control arm, the results must be considered in the context of known limitations of this study design, which the authors acknowledge. Additionally, the study measured results only up to 6 months’ post-procedure, and the authors note that nerve regeneration, which has been observed in animal models, may occur and alter long-term effects. Nonetheless, the excellent safety profile, albeit in a small non-randomized sample set, and decreased HOMA-IR, plasma glucose, liver function tests, and de-escalation in diabetic medications is promising. If reproducible results can be elicited from randomized control trials performed by experienced groups, there will be demonstrable utility for this technique either as a standalone treatment or in a combination with pharmacologic therapy for medication de-escalation. This an encouraging research space because it offers an exciting new role for Interventional Radiologists in treating diseases with a growing public health burden in a potentially single-session, minimally invasive manner.
Additional Reading:
Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension. 2011 May;57(5):911-7. doi: 10.1161/HYPERTENSIONAHA.110.163014. Epub 2011 Mar 14. PMID: 21403086.
Summary
The study enrolled 11 patients with DM2 seeking to improve glycemic control via endovascular denervation of the celiac and peri-celiac sympathetic postganglionic nerves, which suppresses insulin secretion from pancreatic β islet cells. This treatment methodology is based on animal study that showed improved glucose tolerance in rats after celiac ganglionectomy, as well as incidental clinical results in a subset of cancer patients treated with postganglionic nerve block who developed improved glycemic control. The study enrolled patients aged 18-75 with DM2 for at least 5 years, using at least one form of diabetic medication, with the majority of patients using insulin. A 6-electrode radiofrequency endovascular catheter was used to target and ablate the post-ganglionic sympathetic nerves at the celiac and superior mesenteric ganglia. Using a transfemoral approach, an aortogram was performed to position the catheter at the level of the celiac artery and superior mesenteric artery. The EDN device was then deployed, and allowed to ablate for 3 cycles of 120 seconds each at a temperature of 60 degrees Celsius, with a maximum impedance of 400 Ω, after which a completion arteriogram was performed to ensure no vascular injury.
All of the participants achieved technical success, and there were no cases of vascular injury. Approximately 36% of patients developed immediate arterial vasospasm, which resolved shortly thereafter, while a few others developed self-limiting nausea and vomiting, abdominal distention, or constipation. Six-month follow-up demonstrated a significant decrease in the mean HbA1c by 1.9% as well as a significantly decreased homeostasis model assessment of insulin resistance (HOMA-IR) from 13.3 (IQR 5.9-46.1) to 6.0 (IQR 3.1-11.9). Mean fasting plasma glucose also decreased, and 36.4% of patients were able to discontinue at least 1 class of diabetic medication. Weight and body mass index did not undergo significant change, however there was significant decrease in alanine aminotransferase (baseline mean 31.0 IU/L to 24.0 IU/L at 6 months) and gamma glutamyl transpeptidase levels (baseline mean 47.0 IU/L to 27.0 IU/L at 6 months). These reductions suggest an additional modulating effect of EDN on nonalcoholic fatty liver disease (NAFLD), consistent with a recent animal study showing that manipulation of hepatic sympathetic innervation may be a novel therapeutic strategy for NAFLD.
Commentary
The Centers for Disease Control and Prevention estimates that nearly 1 in 10 Americans have diabetes, making it a disease with significant epidemiologic burden and many associated health complications. Thus, any novel treatment to alleviate this immense, growing public health burden could be hugely impactful. Endovascular denervation has been gaining traction in treating another prevalent disease, specifically resistant/refractory hypertension (HTN). This technique is a minimally invasive descendant of surgical sympathectomy for the same indication, which was promising but seemed overly invasive in the face of evolving pharmaceutical therapies. Thus far, results in randomized control trials of renal denervation (RDN) have been promising but mixed, some of which may be attributable to operator inexperience with the technique. Since hypertension and DM2 are frequently comorbid diseases, studies were able to assess the role of RDN in DM2 and showed early promise for achieving glycemic control. However further studies have not shown reliable success for denervation of the renal arteries.
This study by Pan et al. coopts this technique in a different anatomic location, the celiac and peri-celiac aorta, with early promising results as an endovascular approach to achieving glycemic control in patients with DM2. Given that this is a small, nonrandomized study without a control arm, the results must be considered in the context of known limitations of this study design, which the authors acknowledge. Additionally, the study measured results only up to 6 months’ post-procedure, and the authors note that nerve regeneration, which has been observed in animal models, may occur and alter long-term effects. Nonetheless, the excellent safety profile, albeit in a small non-randomized sample set, and decreased HOMA-IR, plasma glucose, liver function tests, and de-escalation in diabetic medications is promising. If reproducible results can be elicited from randomized control trials performed by experienced groups, there will be demonstrable utility for this technique either as a standalone treatment or in a combination with pharmacologic therapy for medication de-escalation. This an encouraging research space because it offers an exciting new role for Interventional Radiologists in treating diseases with a growing public health burden in a potentially single-session, minimally invasive manner.
Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension. 2011 May;57(5):911-7. doi: 10.1161/HYPERTENSIONAHA.110.163014. Epub 2011 Mar 14. PMID: 21403086.
Post Author
Surbhi B. Trivedi, MD
Diagnostic Radiology Resident (PGY-3)
Department of Diagnostic Radiology
University of Illinois Hospital and Health Sciences System
Chicago, Illinois
Twitter: @surbhitrivedi3
Surbhi B. Trivedi, MD
Diagnostic Radiology Resident (PGY-3)
Department of Diagnostic Radiology
University of Illinois Hospital and Health Sciences System
Chicago, Illinois
Twitter: @surbhitrivedi3
Edited and formatted by @NingchengLi
Interventional Radiology Resident
Dotter Institute, Oregon Health and Science University
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.